Private and Public Healthcare: Performance and Privatization
Duarte Miguel Siquenique

Medical Doctor at ULS Santa Maria
17th April 2024
"Privatization almost always led to worse health outcomes, higher avoidable mortality rates and higher hospital infection rates."
Figure 1 – Health Expenditure as a Share of GDP, selected countries, 2006-22 (OECD Health Statistics, 2023, 2023)
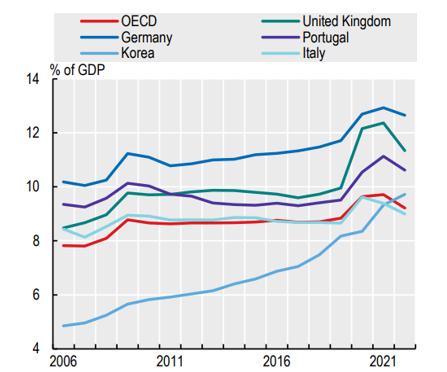
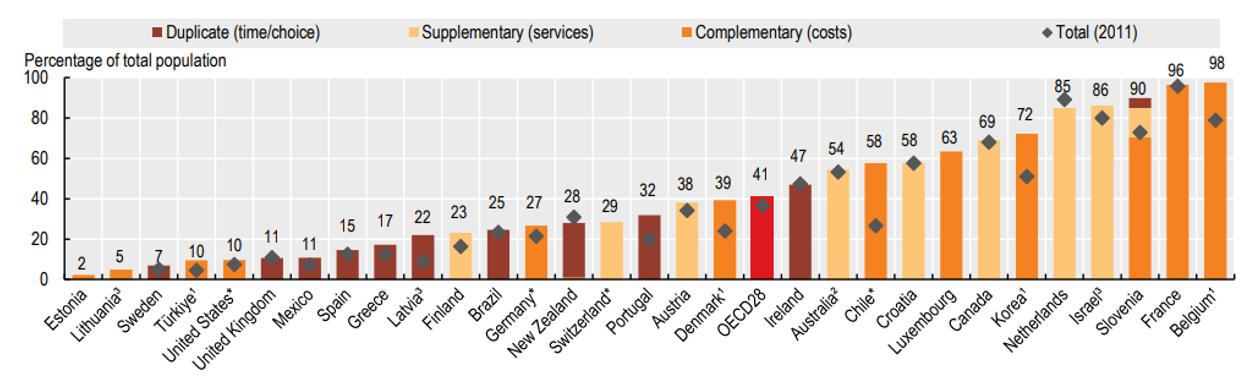
Figure 2 – Voluntary Private Health Insurance Coverage by Type, 2021 and 2011 (or nearest years) (Health at a Glance 2023, 2023)
It begs the question, while perceptions of the inadequacies of the public health service in the last few years have risen, does the private service offer better care? Will privatization of the public health service be for the benefit of society?
Between advocates of public healthcare and private healthcare one idea remains constant: the belief that the better health system is the one that performs the best, be that cost, accessibility, or efficiency. The disagreement comes from which system is better equipped to achieve those goals. Partisans of private systems will argue that the private system is more efficient while their opponents might argue that not having a public health system will leave many undertreated (Basu et al., 2012).
Arguments might get across different viewpoints but are not fact based in and of themselves. For that, let us see what recent peer-reviewed studies have concluded.
Older published research agreed that tighter regulation was necessary to ensure that private healthcare was accessible to all and not only to wealthy users, but a lack of evidence was also a limiting factor in recommending private or public healthcare to achieve health outcomes (Morgan et al., 2016).
Regarding efficiency and quality of care, scientific publications appear to have identified a disconnect between perceptions and measurable impact. In a study conducted on perceptions on the quality of care provided in newly privatized hospitals in Saudi Arabia, patients were more likely to report higher rates of satisfaction with their experiences. Nevertheless, the study didn’t measure actual outcomes, only perceptions (Alumran et al., 2021).
In contrast, a recent review published in The Lancet Public Health (last month) analysing the effects of healthcare privatization in high income countries (as defined by the OECD) was much more assertive in its conclusions. Privatization almost always led to worse health outcomes, higher avoidable mortality rates and higher hospital infection rates. Staffing, particularly skilled nursing staff, was lower in private institutions when compared to before privatization. Regarding accessibility, hospitals became less accessible to patients with less profitable conditions, but more accessible in terms of ease of care (e.g., precise appointments or by telephone) (Goodair et al., 2024).
Even in low- and middle-income countries the private sector appears to have lower efficiency than the public sector (due to for example unnecessary testing and greater risk of complications) while the public sector lacked responsiveness and supplies (Basu et al., 2012).
Another matter is the existence of Public-Private Partnerships. Long seen as a means of providing higher levels of care at a lower cost, the scientific evidence doesn’t appear to be so certain. A recent review of Public-Private Partnerships in Primary Health Services (that is healthcare accessible to anyone, an example in our country is the “Centro de Saúde” or “Médico de Família”) found that they could improve accessibility, especially in more rural areas (Joudyian et al., 2021) but conditional on the ability of public institutions to thoroughly regulate their activities. Another review based on the Portuguese model found that Public-Private partnerships in hospitals were at least equivalent to the care provided in public hospitals (Ferreira & Marques, 2021).
In short, to answer the initial questions: the private service does sometimes offer comparable care to the public service, but at the expense of accessibility (especially in regard to affordability).
References
Alumran, A., Almutawa, H., Alzain, Z., Althumairi, A., & Khalid, N. (2021). Comparing public and private hospitals’ service quality. Journal of Public Health (Germany), 29(4), 839–845. https://doi.org/10.1007/S10389-019-01188-9/FIGURES/2
Basu, S., Andrews, J., Kishore, S., Panjabi, R., & Stuckler, D. (2012). Comparative Performance of Private and Public Healthcare Systems in Low- and Middle-Income Countries: A Systematic Review. PLOS Medicine, 9(6), e1001244. https://doi.org/10.1371/JOURNAL.PMED.1001244
Ferreira, D. C., & Marques, R. C. (2021). Public-private partnerships in health care services: Do they outperform public hospitals regarding quality and access? Evidence from Portugal. Socio-Economic Planning Sciences, 73, 100798. https://doi.org/10.1016/J.SEPS.2020.100798
Goodair, M. B., Goodair, B., & Reeves, A. (2024). The effect of health-care privatisation on the quality of care. The Lancet Public Health, 9, e199–e206. https://doi.org/10.1016/S2468-2667(24)00003-3
Health at a Glance 2023. (2023). OECD. https://doi.org/10.1787/7a7afb35-en
Joudyian, N., Doshmangir, L., Mahdavi, M., Tabrizi, J. S., & Gordeev, V. S. (2021). Public-private partnerships in primary health care: a scoping review. BMC Health Services Research, 21(1), 1–18. https://doi.org/10.1186/S12913-020-05979-9/TABLES/4
Morgan, R., Ensor, T., & Waters, H. (2016). Performance of private sector health care: implications for universal health coverage. In The Lancet (Vol. 388, Issue 10044, pp. 606–612). Lancet Publishing Group. https://doi.org/10.1016/S0140-6736(16)00343-3
